Ensuring equitable healthcare delivery has become a critical issue in today’s global landscape, as vast disparities in access to medical services continue to persist, particularly in developing countries. These nations, which often contend with widespread poverty, face a range of challenges that significantly hinder their ability to provide adequate healthcare. Limited financial resources, underdeveloped infrastructure, and a severe shortage of trained healthcare professionals exacerbate the problem, leaving large segments of the population without access to basic medical services. The COVID-19 pandemic further exposed and amplified these vulnerabilities, demonstrating the urgent need for reform and the adoption of innovative strategies to improve healthcare access, resilience, and quality in underserved regions.
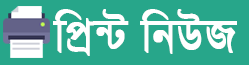
The disparity in healthcare is often most acute in rural and remote areas of developing countries, where health facilities are sparse or non-existent. Residents in these areas frequently must travel long distances to receive even basic medical attention, and the lack of infrastructure, such as roads and transportation, makes this difficult, especially in emergencies. Moreover, healthcare facilities in these regions are often under-equipped and understaffed, with overburdened medical professionals struggling to serve a large patient population.
In many cases, the lack of healthcare professionals is a direct result of the “brain drain,” where doctors, nurses, and other skilled workers leave their home countries in search of better opportunities abroad, further depleting the already scarce workforce. These countries also face the additional challenge of providing adequate healthcare to a growing population while dealing with high rates of infectious diseases like malaria, tuberculosis, and HIV/AIDS, as well as rising incidences of non-communicable diseases such as diabetes, hypertension, and heart disease. This dual burden places an enormous strain on their health systems, making it difficult to prioritize long-term health improvements over immediate crises.
This report delves into new strategies aimed at improving healthcare equity in developing countries, addressing the root causes of healthcare disparities and exploring how international cooperation, advanced technology, and sustainable financing models are driving transformative changes in global healthcare. While the challenges are formidable, emerging solutions—such as telemedicine, mobile health clinics, and public-private partnerships—hold the promise of providing more equitable healthcare services to millions of people in need.
Additionally, with the global push towards achieving Universal Health Coverage (UHC) by 2030, as set out in the United Nations’ Sustainable Development Goals (SDGs), the need to adopt comprehensive healthcare reforms in developing nations is more urgent than ever. This report also examines how UHC frameworks, paired with strategic international funding and capacity-building efforts, can address the financial barriers that prevent millions of people from accessing essential healthcare services.
The COVID-19 pandemic underscored the importance of health equity, revealing stark differences in healthcare access and exposing the vulnerability of health systems worldwide. In response, governments and international organizations have begun to focus more intently on strategies that could close the gap between the healthcare-rich and healthcare-poor, aiming to prevent such global disparities from reoccurring in the future. Through a coordinated and sustained effort, developing countries can enhance their health infrastructure, ensure a more even distribution of medical services, and improve the overall health outcomes for their populations.
This comprehensive exploration not only highlights the ongoing issues but also showcases the innovative approaches and future opportunities for addressing healthcare inequalities, creating a sustainable, fair, and resilient global healthcare system.
Developing countries face numerous obstacles when it comes to providing quality healthcare. These challenges are often interconnected, creating a cycle that perpetuates inequality. Some of the major barriers include:
- Lack of Infrastructure: Rural and remote areas in many developing countries suffer from a lack of healthcare facilities, making it difficult for populations to access even basic medical services. Poor road networks and transportation also hinder patients’ ability to reach existing health centers.
- Human Resource Shortages: Many developing countries experience severe shortages of healthcare professionals, including doctors, nurses, and specialists. This shortage is exacerbated by the brain drain, where skilled workers migrate to higher-income countries for better opportunities.
- Inadequate Funding: Healthcare systems in developing nations are often underfunded, resulting in poorly equipped hospitals, insufficient medical supplies, and limited healthcare programs. Inadequate government spending on health contributes to this issue, alongside challenges in attracting private investment.
- High Disease Burden: Many developing nations are burdened with a high prevalence of infectious diseases, such as malaria, tuberculosis, and HIV/AIDS. This, coupled with rising rates of non-communicable diseases (NCDs) like diabetes and heart disease, overwhelms fragile health systems.
Innovative Strategies for Equitable Healthcare Delivery
In response to these challenges, a number of innovative approaches are being adopted to improve healthcare access and delivery in developing countries:
- Telemedicine and Digital Health: The use of telemedicine has gained significant traction as a means to bridge the gap between rural populations and healthcare providers. Mobile health (mHealth) initiatives are providing essential services such as remote consultations, diagnostic support, and health education. These technologies reduce geographical barriers and allow for better management of chronic conditions and emergency care.
- Task Shifting: Task shifting involves redistributing healthcare tasks from highly qualified healthcare professionals to less specialized staff. This strategy has proven effective in increasing healthcare capacity, especially in rural and underserved areas. For example, community health workers (CHWs) are trained to provide basic medical care, such as administering vaccinations and managing minor illnesses, thus alleviating the workload on doctors and nurses.
- Mobile Clinics and Outreach Programs: Mobile clinics and outreach programs bring healthcare services directly to underserved communities. These initiatives often provide vaccinations, maternal and child health services, and basic medical care. In many instances, they serve as a critical lifeline for communities far from established health facilities.
- Public-Private Partnerships (PPPs): Collaborations between governments, private companies, and non-governmental organizations (NGOs) are proving successful in delivering healthcare services. PPPs can leverage private sector resources and expertise to enhance healthcare infrastructure, provide medical supplies, and extend health insurance coverage to marginalized populations.
The Role of International Cooperation
Global health equity cannot be achieved without strong international collaboration. Organizations such as the World Health Organization (WHO), the World Bank, and global health initiatives like the Global Fund to Fight AIDS, Tuberculosis, and Malaria are playing pivotal roles in supporting healthcare systems in developing countries. By providing technical expertise, financial resources, and capacity-building support, these entities are helping to strengthen healthcare infrastructure and expand access to life-saving treatments.
International cooperation has also been critical in ensuring vaccine equity, especially during the COVID-19 pandemic. Initiatives such as COVAX have sought to distribute vaccines equitably across the globe, though challenges remain in reaching the most vulnerable populations. Moving forward, the international community must continue to advocate for equal access to healthcare resources, focusing on long-term investments rather than short-term relief. In addition, fostering partnerships between developed and developing nations can help bridge the gap in medical research, innovation, and technology transfer. Sustainable global health equity will only be achieved through a united effort to address systemic healthcare disparities and promote inclusive, resilient healthcare systems for all populations.
Sustainable Financing Models
Financing remains a key challenge for healthcare systems in developing countries. Traditional donor-dependent models are proving unsustainable, necessitating the exploration of alternative financing mechanisms. Some emerging models include:
- Universal Health Coverage (UHC) Schemes: Many countries are working toward implementing UHC, which aims to provide financial protection and access to essential health services for all citizens. By pooling funds from government budgets, insurance schemes, and international donors, UHC can help spread the financial risk associated with healthcare.
- Microinsurance Programs: In some developing regions, microinsurance programs are being implemented to provide low-income families with affordable access to healthcare services. These programs allow individuals to pay small, regular premiums in exchange for coverage of essential health services, reducing the financial burden of unexpected medical expenses.
- Innovative Taxation: Some countries are exploring the use of innovative taxation to raise additional revenue for healthcare. For example, taxes on tobacco, alcohol, and sugary beverages are not only a means of discouraging unhealthy behaviors but also a source of funding for public health programs.
The Path Forward: Sustainable Healthcare for All
While significant progress has been made in improving healthcare delivery in developing countries, much work remains. Achieving health equity will require sustained investment in healthcare systems, capacity building, and the implementation of innovative solutions tailored to the unique challenges faced by these countries. This includes not only the development of infrastructure but also investing in healthcare workers, ensuring they have the necessary training and resources to provide high-quality care.
Governments must prioritize healthcare as a key pillar of development and work in collaboration with the private sector, NGOs, and international organizations to ensure that healthcare is accessible to all. Strengthening supply chains for essential medicines and healthcare products, along with implementing digital health solutions, can also play a critical role in reaching underserved populations. Moreover, policies that focus on preventive care, health education, and addressing the social determinants of health will be essential in fostering long-term resilience.
With continued efforts and the adoption of forward-thinking strategies, the vision of equitable healthcare for all is achievable, leading to healthier, more resilient communities across the developing world. A holistic, people-centered approach that empowers local communities to take charge of their health needs will be key in achieving sustainable and equitable healthcare systems for future generations.

 A.B.M. Abir
A.B.M. Abir