The World Health Organization (WHO) has recently unveiled a comprehensive and updated health framework that signifies a pivotal evolution in the approach to primary healthcare (PHC). This new framework is a strategic response to the rapidly shifting landscape of global health challenges and is intended to address a range of complex issues that have emerged in recent years. It aims to bolster health systems globally and advance the goal of Universal Health Coverage (UHC), ensuring that every individual, regardless of their socioeconomic status, has access to essential health services.
The updated framework is meticulously designed to enhance the effectiveness, inclusiveness, and resilience of primary healthcare services worldwide. It takes into account both the existing health issues that continue to challenge health systems and the emerging health threats that require proactive and adaptive strategies. By focusing on improving the quality of primary healthcare, the WHO seeks to create a more equitable and efficient health system that can better meet the needs of diverse populations.
A key aspect of this framework is its emphasis on integrating various levels of healthcare services, ensuring that primary care is well-coordinated with secondary and tertiary services. This integrated approach is intended to facilitate seamless patient transitions across different levels of care and improve overall health outcomes. The framework also underscores the importance of addressing non-communicable diseases (NCDs) through preventive measures, early detection, and effective management within primary care settings.
Moreover, the framework highlights the necessity of addressing health inequities by targeting underserved and marginalized communities, and incorporating strategies that tackle social determinants of health. By fostering community engagement and enhancing the accessibility of services, the WHO aims to reduce health disparities and promote health equity.
In the face of global health emergencies, such as pandemics and natural disasters, the updated framework provides guidance on building resilient health systems capable of responding swiftly and effectively. It emphasizes the role of digital health technologies and innovative solutions in expanding access to care and improving health service delivery.
Overall, the WHO’s new health framework represents a significant advancement in the global approach to primary healthcare. It reflects a comprehensive strategy designed to address current and future health challenges, promote health equity, and strengthen health systems worldwide. By implementing these updated guidelines, the WHO aims to achieve a more inclusive, effective, and resilient healthcare system that can adapt to the evolving needs of populations around the globe.
- Universal Health Coverage (UHC):
- Goal: To ensure that every individual has access to essential health services without experiencing financial hardship. This involves providing a comprehensive range of health services that are affordable and available to everyone.
- Strategies:
- Financial Protection: Implementing health financing mechanisms to reduce out-of-pocket expenses and prevent catastrophic health spending.
- Service Expansion: Increasing the availability of essential health services, including maternal and child health, mental health, and chronic disease management.
- Equitable Access: Addressing barriers to healthcare access in underserved and marginalized populations.
- Integrated Health Services:
- Goal: To offer coordinated and continuous care that integrates various levels of healthcare services and sectors, improving overall patient outcomes and system efficiency.
- Strategies:
- Coordination and Integration: Enhancing collaboration between primary, secondary, and tertiary care providers to ensure seamless patient transitions.
- Multidisciplinary Teams: Utilizing a range of healthcare professionals, including doctors, nurses, pharmacists, and social workers, to provide holistic care.
- Digital Health Technologies: Implementing electronic health records (EHRs), telemedicine, and health information systems to support integrated service delivery.
- Focus on Non-Communicable Diseases (NCDs):
- Goal: To address the growing burden of NCDs, such as cardiovascular diseases, diabetes, cancer, and chronic respiratory conditions, which now constitute a major health challenge globally.
- Strategies:
- Preventive Measures: Promoting healthy lifestyles through public education on diet, physical activity, and tobacco cessation.
- Early Detection: Implementing screening programs and early intervention strategies to manage NCDs effectively.
- Chronic Disease Management: Integrating NCD care into primary health services and providing continuous support for patients with chronic conditions.
- Health Equity and Inclusiveness:
- Goal: To reduce health disparities and ensure that all individuals, regardless of socioeconomic status, gender, ethnicity, or geographic location, have equal access to healthcare services.
- Strategies:
- Targeted Interventions: Developing programs tailored to the needs of underserved communities, including rural populations and marginalized groups.
- Community Engagement: Involving local communities in health decision-making processes and ensuring that services are culturally and contextually relevant.
- Addressing Social Determinants: Tackling factors such as poverty, education, and living conditions that influence health outcomes.
- Resilience to Health Emergencies:
- Goal: To build robust health systems capable of effectively responding to and recovering from health emergencies, including pandemics, natural disasters, and other crises.
- Strategies:
- Emergency Preparedness: Developing and testing emergency response plans, including stockpiling essential supplies and training healthcare workers.
- Surveillance Systems: Enhancing disease surveillance and early warning systems to detect and respond to outbreaks quickly.
- Supply Chain Resilience: Strengthening logistics and supply chains to ensure the availability of critical health supplies and equipment during emergencies.
- Digital Health Innovations:
- Goal: To leverage technology to improve the delivery, accessibility, and efficiency of health services, and to address gaps in healthcare access.
- Strategies:
- Telemedicine Expansion: Increasing the use of telehealth services to provide remote consultations, especially in rural and underserved areas.
- Health Information Systems: Implementing digital platforms for managing patient data, tracking health outcomes, and facilitating communication among healthcare providers.
- Mobile Health Applications: Developing and promoting mobile apps that support health monitoring, self-care, and patient education.
Recent Advances and Implementations
- COVID-19 Pandemic Response: The pandemic has highlighted the crucial role of primary healthcare in managing global health crises. WHO’s updated framework incorporates lessons from the pandemic, emphasizing the need for rapid response capabilities, effective vaccination campaigns, and robust public health communication strategies.
- Mental Health Integration: Recognizing the growing importance of mental health, the new framework includes strategies for integrating mental health services into primary care settings. This approach aims to provide comprehensive care and address mental health issues alongside physical health needs.
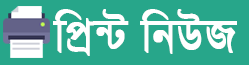
- Community Health Workers: WHO has underscored the role of community health workers in expanding access to care and addressing health disparities. The updated framework includes provisions for training and supporting these workers, who are instrumental in delivering essential services in remote and underserved areas.
Challenges and Future Directions
- Implementation Barriers: While the new framework sets ambitious goals, challenges such as limited financial resources, inadequate healthcare infrastructure, and political instability may hinder its implementation. Addressing these barriers requires coordinated efforts from governments, international organizations, and civil society.
- Monitoring and Evaluation: Effective implementation of the framework necessitates robust monitoring and evaluation systems to assess progress, identify gaps, and make necessary adjustments. WHO will work with member states to develop and utilize these systems to ensure accountability and continuous improvement.
- Global Cooperation: Achieving the goals of the new health framework requires global collaboration and solidarity. WHO’s framework calls for enhanced cooperation among countries, international organizations, and stakeholders to address shared health challenges and achieve common objectives.
The WHO’s new health framework represents a significant advancement in the approach to primary healthcare, addressing contemporary health challenges and promoting equity and inclusiveness. By focusing on Universal Health Coverage, integrated services, health equity, and resilience, the framework provides a comprehensive strategy for strengthening health systems globally. Successful implementation will depend on overcoming challenges, fostering global cooperation, and ensuring that the benefits of these advancements reach all individuals, regardless of their location or socioeconomic status. Through continued dedication and collaborative efforts, the goals of the new framework can be realized, leading to improved health outcomes and a more equitable and resilient global health system.

 A.B.M. Abir
A.B.M. Abir